You don’t know what it is to be an advocate until you are one.
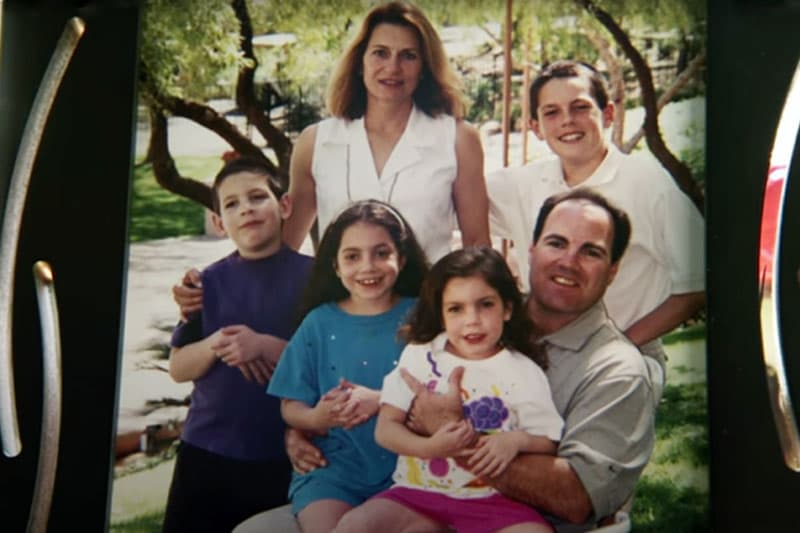
That was never more clear to Harry and Gail Koujaian than when their 5-year-old daughter, Hayley, began having difficulty with motor function, verbal communication, and sight words. Then she had her first seizure.
It took six years of patient advocacy—challenging inaccurate diagnoses, meeting with doctors, pushing for medical tests, becoming “parent scientists,” scheduling surgeries, and planning regular therapy sessions—before the Koujaians would get the correct diagnosis: Niemann-Pick disease type C.


Niemann-Pick disease type C, or NPC, is an inherited, progressive genetic disorder caused by the body’s inability to transport cholesterol and other fatty substances inside of cells. The result is an irreversible dementia-like disease that affects a child’s ability to walk, talk, swallow, and think. The disorder is very rare, affecting one in 120,000 people, and death typically occurs before or during adolescence.
Hayley was diagnosed with the terminal disorder at the age of 11. Her older brother, Alec, was diagnosed shortly thereafter at 13.
The Koujaian family’s experience is all too common. With more than 7,000 different diseases classified as “rare,” 10 percent of the population is likely to encounter a diagnostic odyssey of unnecessary tests and wrong diagnoses in their push for effective care.
An urgent need
The University of Notre Dame’s Boler-Parseghian Center for Rare and Neglected Diseases has worked with NPC patients since 2008, understanding the importance of patient advocacy in the fight for adequate treatment and health care. Over the last 15 years, as the center has expanded research from one disease to a dozen rare diseases, it has also grown its advocacy efforts via public events, community outreach, and the creation of a new curriculum.
In 2021, the center and Notre Dame’s College of Science launched a minor in science and patient advocacy to provide undergraduate students with critical skills and understanding of the multifaceted challenges needed to advocate effectively for rare disease patients.
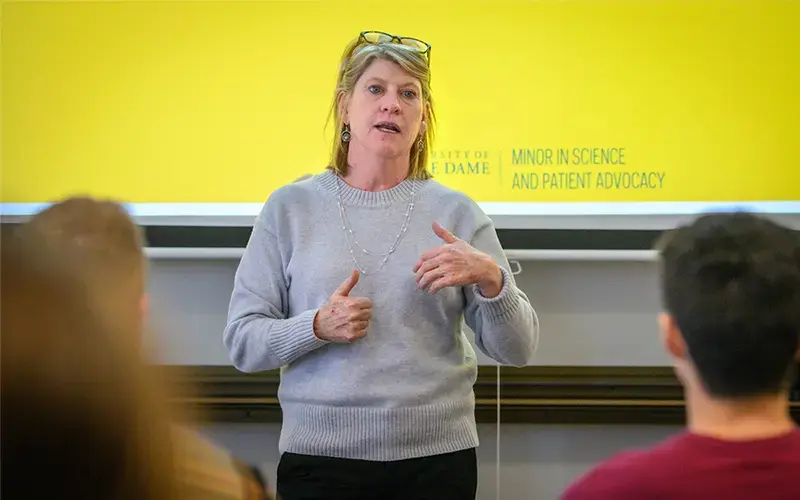
It’s the first patient advocacy program in the country to focus its efforts on supporting the rare disease community. And more than that, the minor provides students hands-on experience to benefit patients and their families.
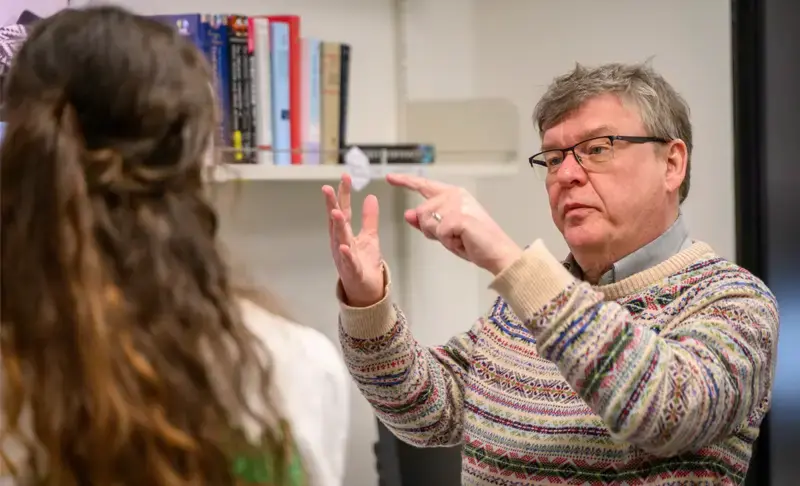
“Patient advocacy is about amplifying the voice of the patient, understanding that the patient and their caregivers are the experts in their disease, and treating them as such. Everyone can do that in whatever role they hold,” said Barb Calhoun, the Reisenauer Family Director for Patient Advocacy Outreach and Education in the College of Science and director of the minor in science and patient advocacy.
While the Clinical Research in Rare Disease course taught by Calhoun starts by teaching the definition of rare disease and patient advocacy, students spend the bulk of the class time working with real NPC patient medical records.
A handful of medical records, voluntarily given and de-identified, are shared with small teams of students who are then charged with compiling a natural history for patients and their families. For participating families, the class creates a summary that streamlines years of medical history, which can be shared with doctors. For the students, it provides a look at the reality of living with a rare disease and the challenges of navigating a cumbersome health care system.
Throughout this process, students in the course keep a symptom list for their patient and develop a better understanding of clinical language.
“It’s really cool to watch as the students transform. At first they will ask you questions about every technical word they read, but eventually they learn the terms and begin using them in class,” Calhoun said. “This is so vital because otherwise students wouldn’t get this kind of exposure.”
The course also works indirectly with rare cancer patients through a collaboration with Dr. Jose Bufill of Michiana Hematology Oncology at Saint Joseph Regional Medical Center. That project works with area patients who have run out of traditional treatment options. As part of the class, students look for potential clinical research and drug trials that patients may be eligible to join. The collaboration provides a platform for students to learn the ins and outs of accessing clinical research in real time.

But the most rewarding aspect of the minor is the direct interaction between students and rare disease patients. It’s an opportunity for families, like the Koujaians, to share the nuances and challenges that students may one day be able to help address. And with the new Patient Partnership Program launching in 2024, students will have even more access to other rare disease patient families.
“The minor really opened my eyes to this whole other world,” said Jake Weber, a senior pursuing a minor in science and patient advocacy. “You get to see it from two different perspectives: the community and the patient side, which was my favorite part, and the industry side. I learned all of that through a lens of rare disease and patient advocacy, which I would not have gotten if I hadn’t joined the minor.”
In 2022, the College of Science received a founding gift from Horizon Therapeutics (now Amgen) and an additional gift from Dyne Therapeutics to found the Patient Advocacy Initiative to support more programming at Notre Dame like the minor that advances training, outreach, and research to serve the rare disease community.
So far 13 students have graduated from the minor in science and patient advocacy. While some graduates are on track to become doctors or genetic counselors or work in clinical research, all are currently teed up to serve in roles that could benefit rare disease patients and their families.
65 undergraduates enrolled in the patient advocacy minor
20 rare diseases advocated for at the Boler-Parseghian Center
29 patient advocacy program graduates by 2024
>1% or $38M of NIH annual funding supports rare disease research (as of 2019)
300 undergraduates engaged in rare disease research at Notre Dame
$60M in funding from APMRF for NPC research
A doctor who listens
The Koujaian family had worked with three different pediatric neurologists before they went to Rush University Medical Center in Chicago and found Dr. Elizabeth Berry-Kravis, a 1979 alumna of Notre Dame. Prior to meeting Hayley, Berry-Kravis, or “Dr. K” as she is lovingly referred to, had never worked with an NPC patient.
Gail and Harry Koujaian were most interested in her word-of-mouth reputation with families. For years, the Koujaians had struggled to find doctors who were willing to listen to them and their needs. They wanted a doctor who wouldn’t just treat their daughter’s symptoms, but would also help them find a cure for their children.
“NPC causes damage to you every single second, of every single minute, of every single hour, of every single day, of every single year. The progression is going to be different for different kids, but the damage is there and it will always be there, unless we stop it,” Harry Koujaian said.
Berry-Kravis is well-known for her work with fragile X syndrome, another rare disease, and for her experience with clinical research, providing the most promising advances in patient care. When the Koujaians met with her, they were hoping she could help them access cyclodextrin, a drug that was not yet approved.
“At first I thought, ‘Well, this will be a huge amount of work.’ But honestly, I was the only one in Chicago with the kind of clinical experience needed to do this for them,” Berry-Kravis said.



Cyclodextrin, also known as adrabetadex, was being used in a National Institutes of Health natural history study that the Koujaian family was hoping to get Hayley added to. However, after multiple attempts to qualify, she was denied access to the study and therefore, the drug. As a result, Berry-Kravis applied to the FDA for compassionate use authorization of cyclodextrin for Hayley as well as Alec.
“When you’re using a disease directed treatment for a degenerative disease, the patients that it works the best for are those that get treatment early on,” Berry-Kravis said. “So we decided we would also treat Alec, because actually, it might potentially have more benefit for him.”
While the medication slows the progression of disease, it cannot completely stop it.
“Everyone wants a cure, but we are thankful for the medications that give us time and quality of life for our kids,” Gail Koujaian said. “We are thankful for what we have until a cure is found.”
In 2020, Hayley Koujaian passed away at the age of 20 from NPC.
A reason for research
Cindy and Mike Parseghian established the Ara Parseghian Medical Research Foundation in 1994 when three of their four children—Michael, Marcia, and Christa—were diagnosed with NPC. The foundation was merged into the Ara Parseghian Medical Research Fund at Notre Dame in 2016.
By providing approximately $60 million in research grants, the fund is dedicated to finding a treatment for NPC. Most notably, the fund was the lead supporter of the research that identified the NPC1 gene, which causes the disease.
“With the concern, support, and generosity of the Notre Dame community, we have been able to make significant steps in understanding the research and moving therapies along the drug development pathway,” Cindy Parseghian said. “Notre Dame has been a blessing to all NPC patients and their families!”


Another important accomplishment of the fund is its work to bring together NPC families and the researchers studying the disease.
“The support we’ve had from NPC families spearheaded by the Koujaians is incredible,” Cindy Parseghian said. “They keep spreading the word and they have a huge impact on fundraising and on research when they allow their children to be in these clinical trials. That is a big sacrifice. Their commitment has been phenomenal.”
The fund brings together researchers and NPC patient families alike at its annual conference in Arizona. It was at one of these conferences in 2005 that Paul Helquist, professor of chemistry and biochemistry, and Olaf Wiest, the Grace-Rupley Professor of Chemistry and Biochemistry, presented their research and introduced themselves to the NPC community for the first time.

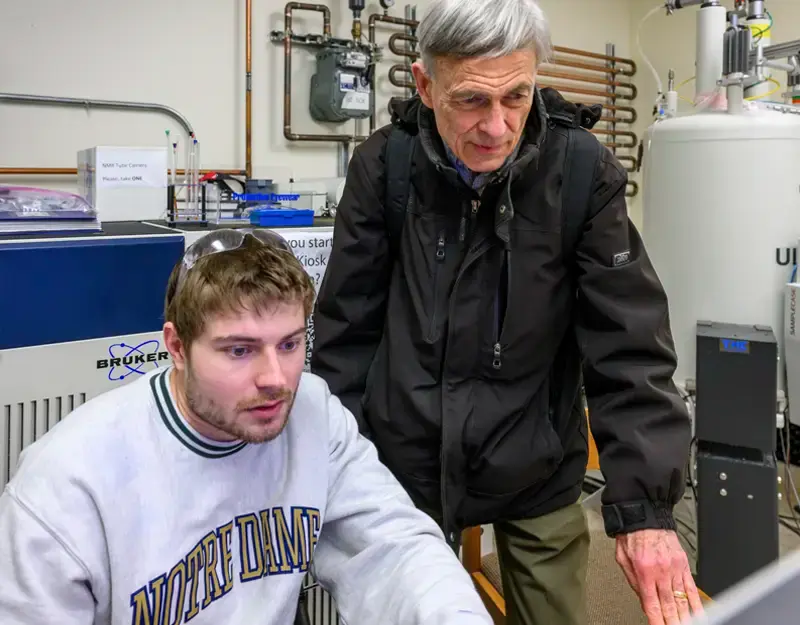
At that event, Helquist and Wiest learned more about the disease and where research currently stood and met afflicted NPC patients and families. It’s also where they were introduced to Fred Maxfield, a professor at Cornell University and an expert in cell biology. That meeting would lead to a decades-long collaboration among the three as they investigated NPC and drug discovery for the disorder.
“Essentially all of the research that had been done at that point was strictly biological to understand the disease. NPC was originally this mystery disease. But Cindy thought there was enough biology understood and that maybe some new medicinal chemistry could be started,” Helquist said. A year later, the researchers applied for their first grant from the fund.
Over the last 20 years, Helquist and Wiest have published numerous studies on the fundamental science behind NPC. Supported by the fund, their research has contributed significantly to the understanding of the NPC1 gene and has been key for identifying potential drug targets.
“It’s hard because everyone—parents, caregivers, and researchers—wants a cure now. But this kind of work takes decades, and with drug trials, there are going to be a lot more failures than successes,” Wiest said.

Cyclodextrin is among the drugs that they are working to improve. Although it has benefited NPC patients, there are still some things the drug can’t do well, such as crossing the blood-brain barrier, a membrane between the blood and the connective tissue of the brain that makes drug delivery into the brain notoriously difficult. A current area of interest for Wiest, Helquist, and Maxfield is looking into a new molecular transport mechanism that may better help the drug get into the brain.
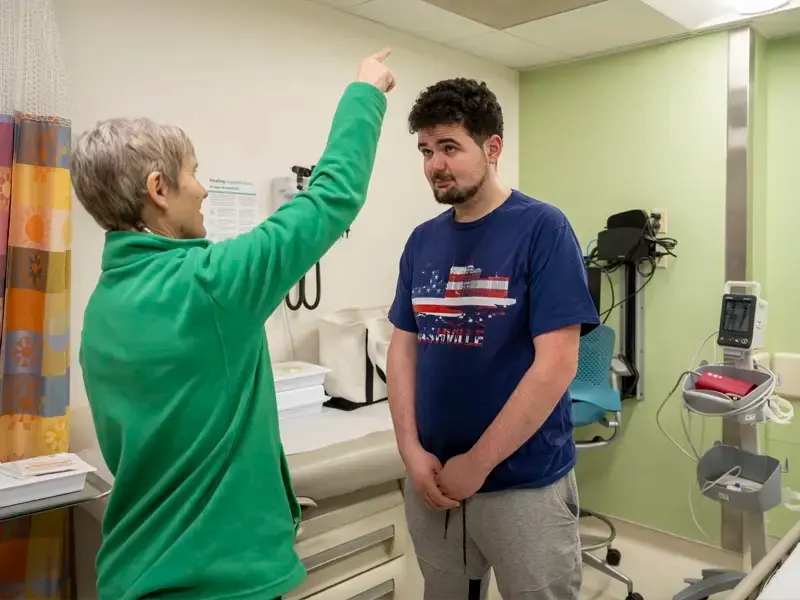
While their research continues, cyclodextrin is still being used for many NPC patients, including those in Berry-Kravis’s expanded access (compassionate use) program. Hayley Koujaian was the first patient in that program, and work continues today by serving 45 NPC patients from across the country, including Alec Koujaian.
Advocacy in action
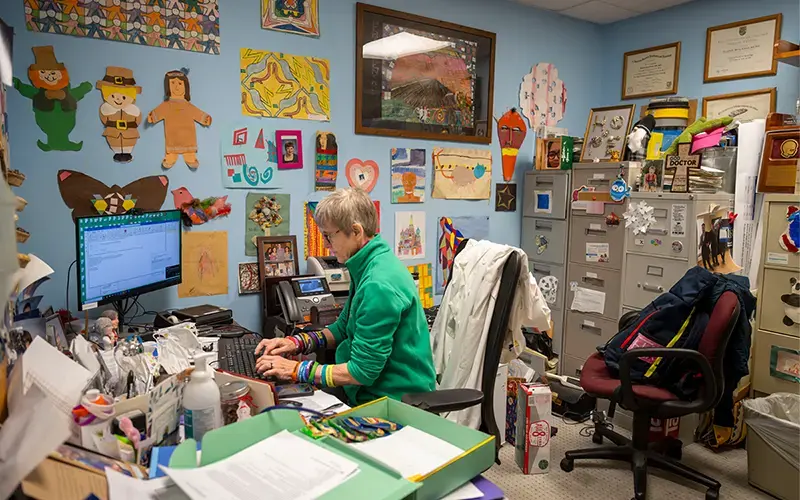
Samantha Dreyer began working for Berry-Kravis after graduating from Notre Dame in 2023 with a bachelor’s degree in neuroscience and a minor in science and patient advocacy. As part of her position as a research coordinator, she supports Berry-Kravis’s research clinics.
Upon meeting a new patient and their family, Dreyer’s first step is to create a good environment and build a relationship.

“If the person that was working with me and treating my child wasn’t interested in my kid beyond their disease, I would feel a little weird. I want the families to feel confident with what we are providing for them,” Dreyer said. “Especially with rare disease. I just want them to know I see them, I hear them, and I understand them.”
Courses required in the minor, such as Clinical Research in Rare Disease, provided Dreyer the real-world clinical experience that she uses every day in her role. Without them, she believes she wouldn’t be as effective at her job.
“Before I started taking those classes, I truly did not know what clinical research was, and that’s my job now,” Dreyer said. “I learned so much about what goes into a study, what happens on the FDA side of things, how you craft a study, what you do during it, the data entry, and the natural history of a disease from Notre Dame.”
Dreyer’s favorite part of the minor was the courses that discussed precision medicine and the importance of effectively tending to patients by tailoring care to them.
Berry-Kravis shared how impressed she’s been by Dreyer’s commitment to the patients and the skill she brings to work each day.
“Sam works very well with families. She bonds with the kids and she loves the kids. Part of that, no doubt, is her personality. But some of it is from her know-how from the patient advocacy program.”
The program’s influence on Dreyer, Berry-Kravis recalled, really shined when a patient’s family requested a support document for their insurance. Normally, that would be something Berry-Kravis would fill out, but Dreyer offered to do it. Berry-Kravis worried that she would have to heavily edit whatever Dreyer wrote. To her surprise, it was exactly what the family needed.


“Coming into a job where you constantly have requests for something patients need, it’s so important to have an idea of why the patients are asking for it, and understanding what they’re advocating for is tremendously valuable,” Berry-Kravis said. “That’s been one of the best supports that Sam has been able to do for me this year.”
What Dreyer has been able to do as a research coordinator is what the minor in science and patient advocacy is all about. Her job has put her in a position to support the advancement of research into rare diseases like NPC while also helping connect patients to much-needed resources.
“One of the things the students in the minor always say is that they want more rare disease patient interaction,” Calhoun said. “And that’s the big thing. The students want to be with patients. They want to learn from them and they want to help them.”
In May, 16 students will graduate from the minor, and 49 other students are currently enrolled. The program has become a magnet for Notre Dame undergraduates wanting to make a difference in the world for patients like Alec Koujaian, who has spent 10 years making visits every other week to Berry-Kravis’s NPC clinic to receive a lumbar puncture that delivers cyclodextrin directly into his nervous system.
Thanks to that treatment, Alec has a full and vibrant life, just like any other young adult. He is quick to joke around with his mom and competitive while video gaming with his dad. He plays in a local basketball league, works at a home improvement retail store, and even finds time to sing karaoke with his friends on the weekend.
At 25 years old, Alec is a vision of hope for all NPC patients.